Getting Started
Important:
For Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members, Michigan’s prior authorization law requires health care providers to submit prior authorization requests electronically.
If you’re experiencing temporary technical problems, such as a power system or internet outage, you can submit requests using other methods.
Submit prior authorization requests
For the fastest response, submit prior authorization requests electronically through our provider portal, Availity® Essentials. Through our provider portal, you can access:
- The e-referral system to submit requests to Blue Cross or BCN
- Prior authorization systems to submit requests to vendors who manage prior authorizations for various services
Follow the appropriate steps to access our provider portal and submit requests:
| Provider's location | Contracted with Blue Cross Blue Shield of Michigan or Blue Care Network? | Steps |
|---|---|---|
| Michigan | Yes |
|
| Outside of Michigan and registered with Availity | Yes |
|
| Outside of Michigan and registered with Availity | No |
|
| Outside of Michigan and not registered with Availity | No |
|
You can find information about submitting prior authorization requests using other methods, such as phone or fax, by looking up information on specific services on this website.
Set favorites for easy access
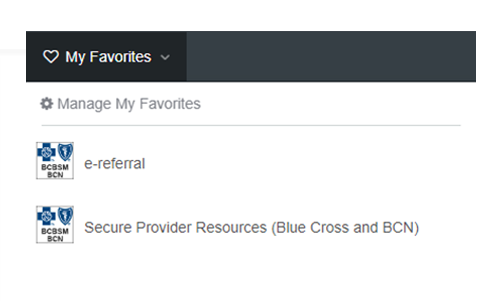
You can click the heart on any tile in the Applications tab to “favorite” it.
1.
The items you favorite appear in My Favorites at the top of the screen. (You can also favorite other items throughout Availity.)
2.
Register for Availity Essentials
You must have a secure user ID and password for our provider portal, Availity Essentials. Your Availity Essentials administrator must set this up for you.
Learn more about the benefits of registering.
Access Prior Authorization Sytems
Once you have access to Availity Essentials, you’ll automatically have access to prior authorization systems.
Set up access to the e-referral system
Your Availity Essentials administrator must take steps to give users access to the e-referral system. For details, see Availity administrators: Set up the e-referral tool![]()
Maintain user access to the e-referral system
Availity Essentials administrators can add or remove practitioners from the scope of a user’s e-referral access. For instructions, see Availity administrators: Set up the e-referral tool![]()
e-referral users must access e-referral at least once every 90 days to keep their user IDs active. If a user who previously had access can no longer access e-referral, they should contact Availity Client Services at 1-800-AVAILITY (1-800-282-4548).
Learn more about the e-referral system
For additional information about working in the e-referral system, refer to the appropriate e-referral User Guide or web-based training.
Remove user access to Availity Essentials
When there are staff changes, Availity Essentials administrators can remove a user’s access to Availity Essentials. For more information, see Availity Essentials administrator guide![]()
Before you can remove an Availity Essentials administrator’s access to Availity Essentials, call Availity Client Services at 1-800-282-4548. They’ll need to change the administrator who is on record before access can be removed.
Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.